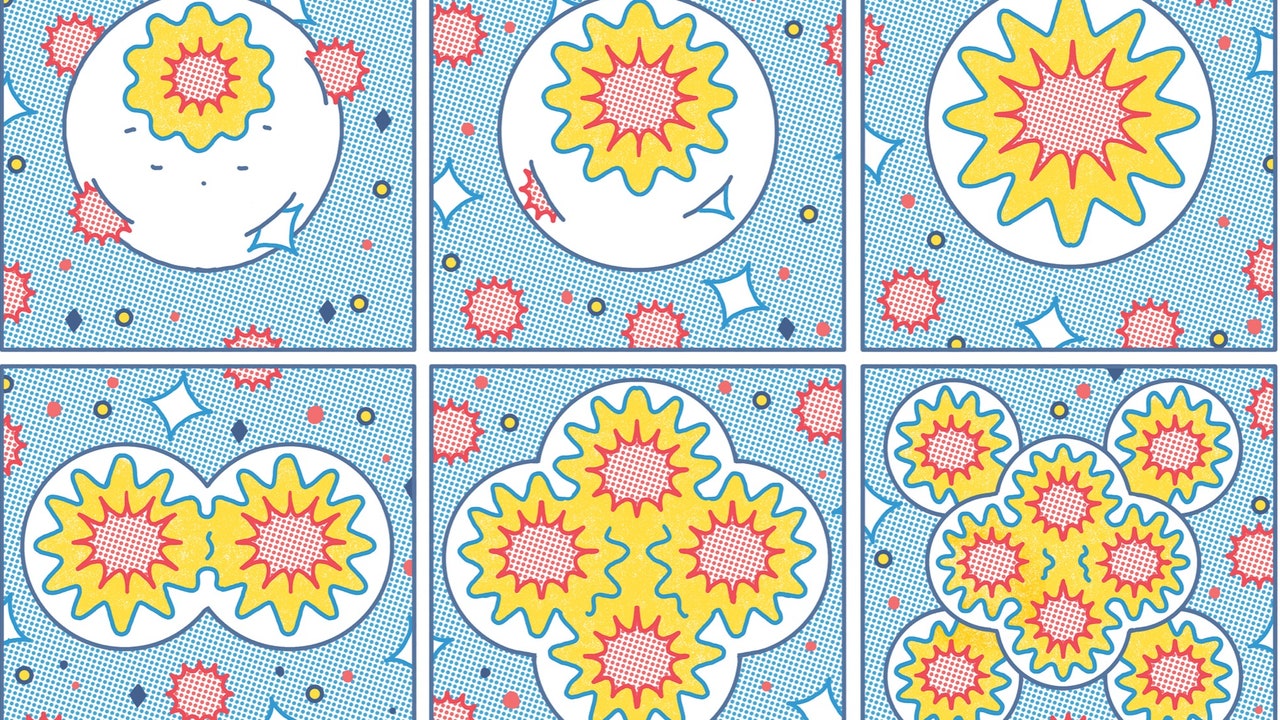
We routinely test for chemicals that cause mutations. What about the dark matter of carcinogens—substances that don’t create cancer cells but rouse them from their slumber?
In the nineteen-seventies, Bruce Ames, a biochemist at Berkeley, devised a way to test whether a chemical might cause cancer. Various tenets of cancer biology were already well established. Cancer resulted from genetic mutations—changes in a cell’s DNA sequence that typically cause the cell to divide uncontrollably. These mutations could be inherited, induced by viruses, or generated by random copying errors in dividing cells. They could also be produced by physical or chemical agents: radiation, ultraviolet light, benzene. One day, Ames had found himself reading the list of ingredients on a package of potato chips, and wondering how safe the chemicals used as preservatives really were.
But how to catch a carcinogen? You could expose a rodent to a suspect chemical and see if it developed cancer; toxicologists had done so for generations. But that approach was too slow and costly to deploy on a wide enough scale. Ames—a limber fellow who was partial to wide-lapel tweed jackets and unorthodox neckties—had an idea. If an agent caused DNA mutations in human cells, he reasoned, it was likely to cause mutations in bacterial cells. And Ames had a way of measuring the mutation rate in bacteria, using fast-growing, easy-to-culture strains of salmonella, which he had been studying for a couple of decades. With a few colleagues, he established the assay and published a paper outlining the method with a bold title: “Carcinogens Are Mutagens.” The so-called Ames test for mutagens remains the standard lab technique for screening substances that may cause cancer.